Readmissions
Overview
Hospital readmissions are one of the most common healthcare concepts. They are also one of the most complicated concepts to define and implement as code. Here we provide a general overview of how to calculate a hospital readmission measure.
There are many different ways to define hospital readmission measures. However every readmission measure is built on two underlying concepts: the index admission and the readmission. The index admission is a hospitalization that qualifies to be included in the readmission measure. Not all hospitalizations will meet the criteria to be index admissions and will therefore not be included in the readmission measure. For example, if a patient dies during a hospitalization, that hospitalization will not be an index admission, and will not be included in the readmission measure. There are many more pieces of logic to define if a hospitalization counts as an index admission for each different readmission measure. For example, hospitalizations for medical treatment of cancer are not index admissions. We explain each piece of logic further below.
To better understand these fundamental concepts, it is helpful to think of building a readmission measure as follows:
- Start with a data table of inpatient admissions, one record per admission.
- Use logic (defined further below) to compute two additional columns which you append to this table:
- The first column (index_admit_flag) is a binary variable that indicates whether each inpatient admission qualifies as an index admission.
- The second column (readmit_flag) is a binary variable that indicates whether each inpatient admission had a subsequent admission that qualifies as a readmission.
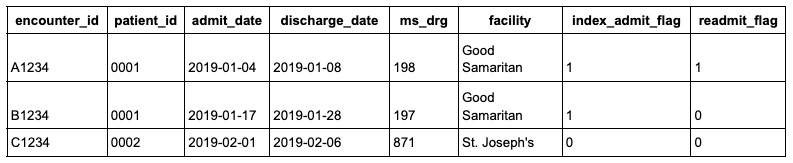
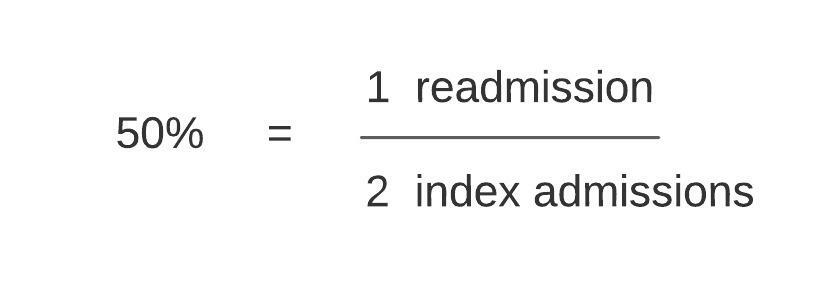
The index admission (index_admit_flag) and readmission (readmit_flag) are then used to compute the readmission measure. The sum of the index_admit_flag column forms the denominator of the readmission measure while the sum of the readmit_flag column forms the numerator. In the example data table above there are 3 total inpatient admissions, 2 index admissions, and 1 readmission, resulting in a 50% readmission rate.
The different definitions of readmission measures are simply variations in the inclusion and/or exclusion criteria that define the index_admit_flag and the readmit_flag. The most commonly used readmission measures are the CMS readmission measures.
There are 7 such measures grouped into 3 categories:
- All-cause Hospital-wide Readmissions (1)
- Condition-specific Readmissions (4)
- Acute Myocardial Infarction
- Congestive Obstructive Pulmonary Disease (COPD)
- Pneumonia
- Heart Failure
- Procedure-specific Readmissions (2)
- Total Hip/Knee Arthroscopy
- Coronary Artery Bypass Graft
CMS Readmissions Algorithm
The All-cause Hospital-wide Readmission Measure (“Hospital-wide Measure”) is the most commonly used readmission measure definition of all. The sections that follow describe how to define and implement the Hospital-wide Measure on EHR data or claims data in your data warehouse. This measure has also been encoded into the Tuva Project, including all necessary terminology datasets and data quality tests.
Data Requirements
The Hospital-wide Measure can be implemented on either EHR data or claims data. Strictly speaking, CMS developed the Hospital-wide Measure to run on Medicare FFS claims data, but CMS explicitly states in their documentation that the measure may be adapted to run against an all-payer patient population.
The data elements needed to process the readmission measure are listed below.
- patient
- person_id
- gender
- birth_date
- encounter
- encounter_id
- person_id
- encounter_start_date
- encounter_end_date
- discharge_disposition_code
- location
- ms_drg
- encounter_type
- condition
- encounter_id
- code
- diagnosis_rank
- code_type
- condition_type
- procedure
- encounter_id
- procedure_code
- code_type
Terminology Datasets
The Hospital-wide Measure requires several terminology datasets that are used as lookup tables to create the index admission and readmission. The following is a complete list of the terminology datasets that are needed:
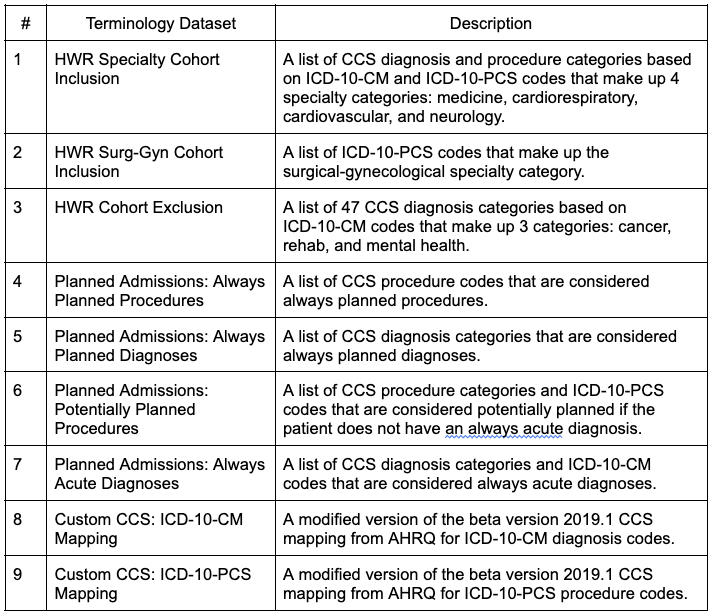
CMS makes these terminology datasets available as files on the quality net website. The links below download two Excel spreadsheets that include all the terminology datasets listed above.
- https://qualitynet.cms.gov/files/60943ca9fd340b002259fe16?filename=2021_HWR.xlsx
- https://qualitynet.cms.gov/files/6092ab86fd340b002259fda0?filename=YaleMod_CCS_PCS_CM_Map_v2020.xlsx
These terminology datasets are already included in the Tuva Project.
Index Admission Algorithm
The index admission algorithm is the set of sub-algorithms (i.e. rules) that together determine whether an inpatient admission qualifies as an index admission (i.e. receives an index_admit_flag = 1 or 0). Not every inpatient admission qualifies as an index admission.
Here are the sub-algorithms used by the Hospital-wide Measure:
- Cohort Inclusion Algorithm
- Cohort Exclusion Algorithm
- Discharged Alive and Not Against Medical Advice
- Not a Transfer
- Not a Same Day Readmission
- Run-out
If an inpatient admission meets the criteria from all of these sub-algorithms then it qualifies as an index admission. Otherwise it does not. Below we walk through each sub-algorithm.
Cohort Inclusion Algorithm
The cohort inclusion algorithm is a set of rules that determine whether an inpatient admission belongs to 1 or more specialty categories. In order to qualify as an index admission, an inpatient admission must belong to 1 or more of these 5 specialty categories:
- Medicine
- Cardiorespiratory
- Cardiovascular
- Neurology
- Surgery / Gynecology
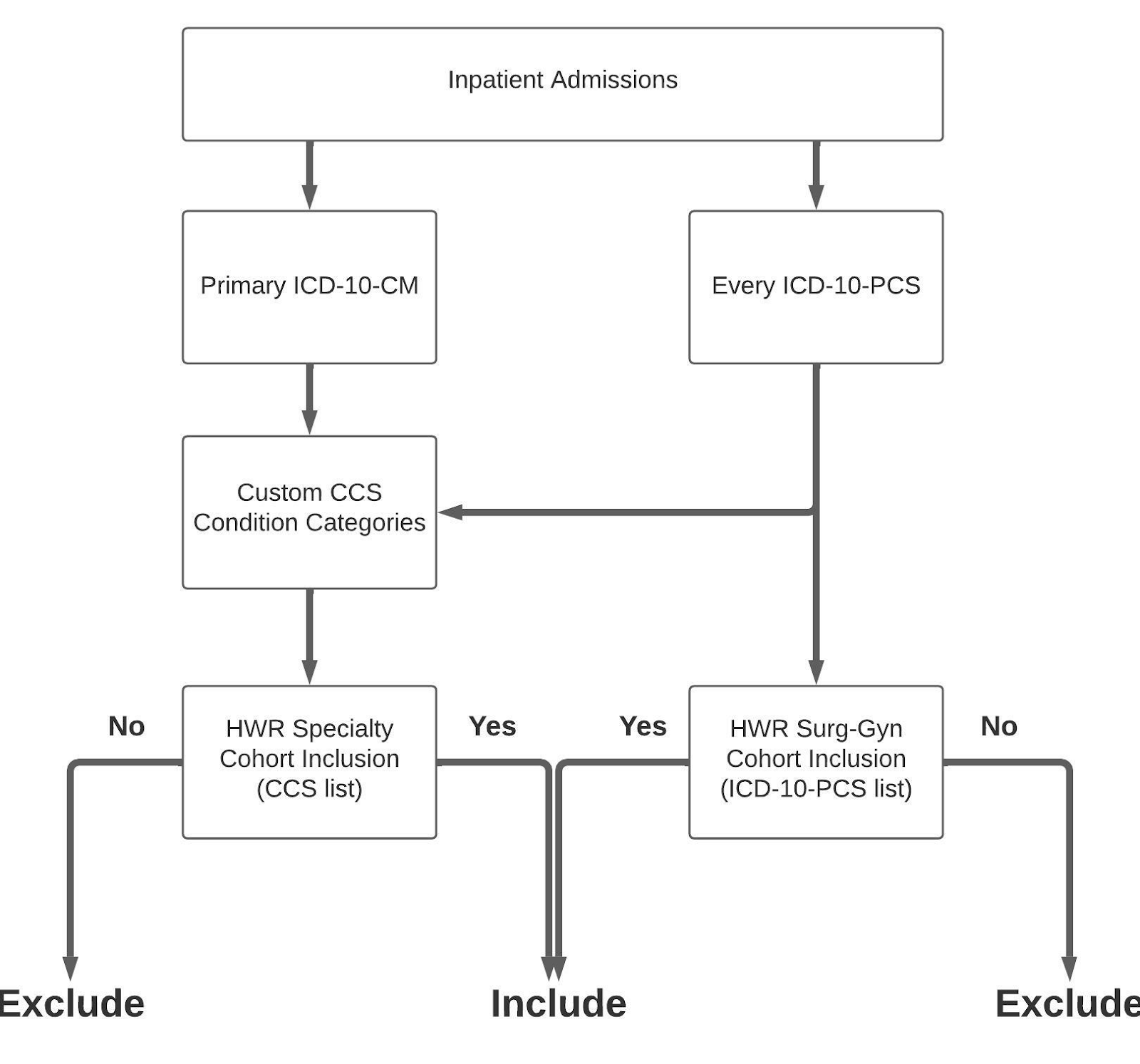
Here are the steps to implement the cohort inclusion algorithm:
-
Each inpatient admission should have 1 primary ICD-10-CM diagnosis code and 0 or more ICD-10-PCS procedure codes associated with it.
-
Map each of these codes to the custom CCS Condition Categories (terminology datasets #8 and #9). Now each inpatient admission should have its corresponding CCS diagnosis and procedure categories assigned.
-
For each inpatient admission, map its assigned CCS diagnosis and procedure categories to those listed in the HWR Specialty Cohort Inclusion terminology dataset (terminology dataset #1) to determine if it should be assigned to any of the first 4 specialty categories (medicine, cardiorespiratory, cardiovascular, and neurology).
-
For each inpatient admission, map its ICD-10-PCS codes to those listed in the HWR Surg-Gyn Cohort Inclusion terminology dataset (terminology dataset #2) to determine if the readmission should be assigned to the Surgical / Gynecology specialty category.
-
Inpatient admissions are successfully assigned to one or more specialty categories based on steps 3 and 4 pass this algorithm. Otherwise the admission fails and is no longer a candidate for an index admission.
Here is a diagram of the cohort inclusion algorithm:
Cohort Exclusion Algorithm
An inpatient admission does not qualify as an index admission if the primary reason for the index admission was related to cancer, rehabilitation, or mental health. These categories are defined in the HWR Cohort Exclusion terminology dataset (terminology dataset #3). In order to use this dataset, first map all primary ICD-10-CM codes to the Custom CCS mapping dataset and then lookup whether each inpatient admission had any of these CCS condition categories.
Inpatient admissions that do not map to any of these CCS condition categories pass this criteria for inclusion as an index admission.
Discharged Alive and Not Against Medical Advice
In order to qualify as an index admission the inpatient admission must not have a discharge status of 20 (‘expired’) or 07 (‘left against medical advice’).
Not a Transfer
Inpatient admissions that result in the patient being transferred to another acute care facility do not count as index admissions. However, the subsequent transfer does count as an index admission if:
- The patient is discharged alive and not against medical advice
- The patient is discharged to a non-acute care setting (e.g. home, SNF, etc.)
Importantly, the transfer does not necessarily have to meet the other index admission criteria. For example, the transfer does not have to pass the cohort inclusion algorithm as long as the initial admission does.
A transfer is defined as occurring if a patient is discharged from an acute care hospital and admitted to another acute care hospital on the same day or the following day. No other criteria such as discharge status or admit source is required to define a transfer.
Not a Same-day Readmission
An inpatient admission is not considered an index admission if the patient is readmitted to the same hospital on the same day they were discharged from a previous admission for the same condition. In this situation, the readmission itself qualifies as the index admission.
Run-out
In order to qualify as an index admission, the admission must occur at least 30 days before the last date of discharge in the dataset.
For example, suppose your dataset contains inpatient admissions that occurred in calendar year 2018. Without this rule, admissions in this dataset that occurred on the last date in the dataset (i.e. December 31, 2018) could be flagged as index admissions but would never have an associated readmission because the data does not exist. As a result the readmission measure for the month of December 2018 would be artificially low (there would be a typical number of index admissions but fewer than typical readmissions simply because the data does not exist).
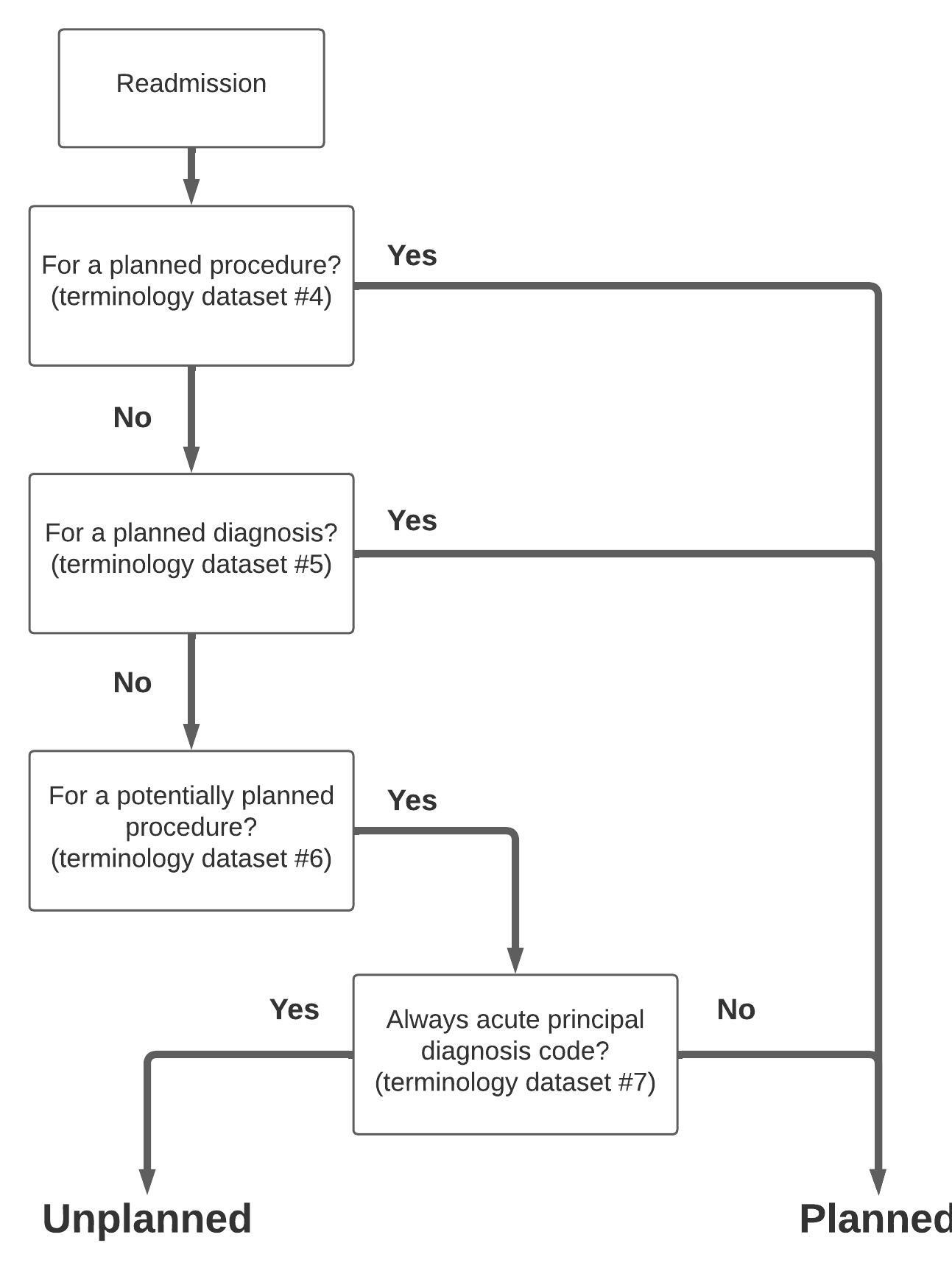
Planned Admission Algorithm
The planned readmission algorithm is used to exclude planned admissions from being flagged as readmissions in the Hospital-wide Measure. Terminology datasets #4-7 are used in this algorithm.
Here are the steps to implement the algorithm:
-
This algorithm requires mapping the primary ICD-10-CM code to the custom CCS diagnosis categories and all the ICD-10-PCS codes to the custom CCS procedure categories for each inpatient admission (terminology datasets #8 and #9).
-
For each inpatient admission, check whether the CCS diagnosis and procedure categories fall under the "always planned" list of diagnoses and procedures (terminology datasets #4 and #5). If any match occurs, this is a planned admission.
-
For each inpatient admission, check whether the CCS procedure categories and ICD-10-PCS codes fall under the list of potentially planned procedures (terminology dataset #6). If any match occurs, check whether this patient had any primary ICD-10-CM code or CCS diagnosis category that is considered an "always acute" code (terminology dataset #7). If the answer is no, this is a planned admission.
-
Inpatient admissions that do not qualify as planned admissions based on steps #2 and #3 above are considered unplanned.
Here is a diagram of the algorithm:
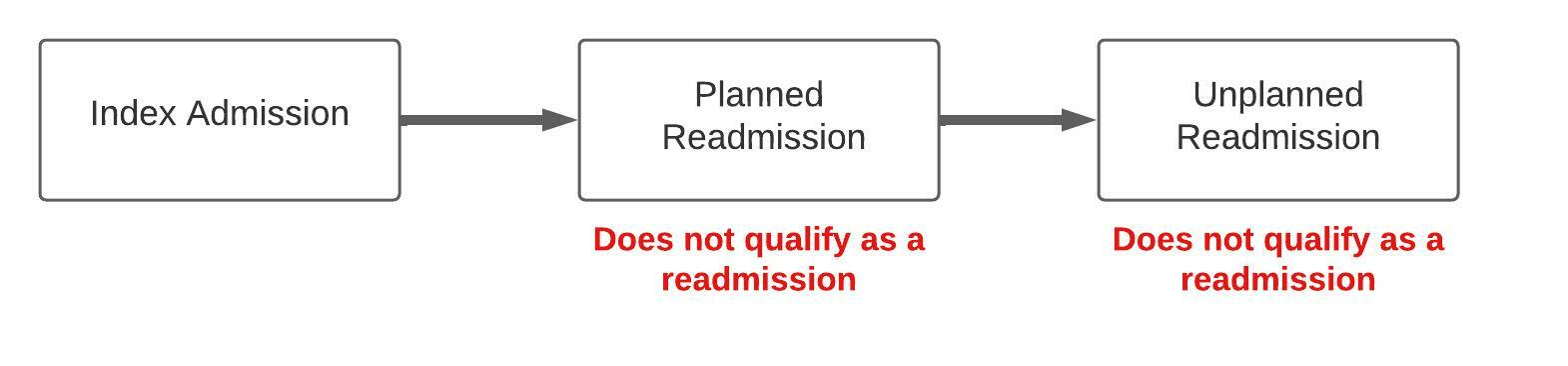
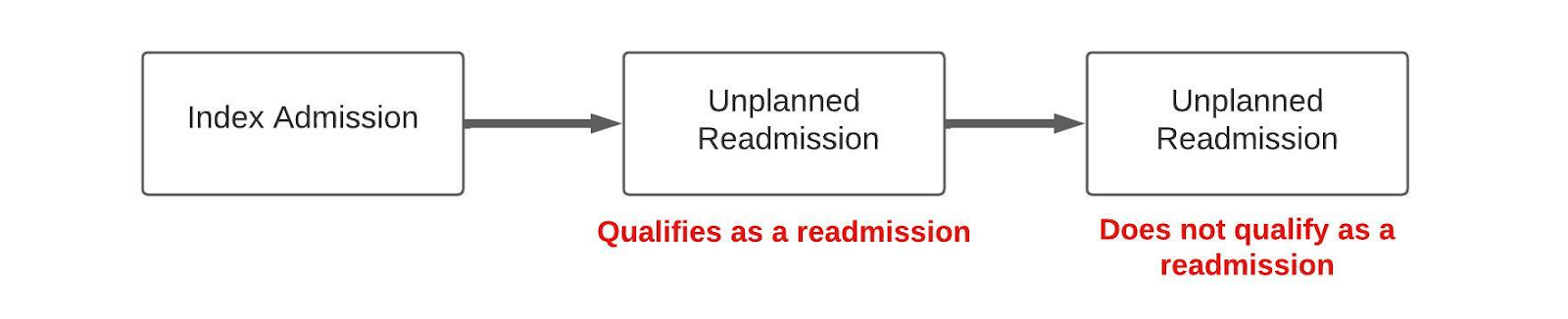
Unplanned Readmission Algorithm
An admission that occurs within 30 days of an index admission is considered a readmission if it meets the criteria below:
- Not a Planned Readmission
- Does Not Follow a Planned Readmission
- Not a Multiple Readmission
Planned readmissions are excluded from the readmission measure, as described in the previous section.
In a chain of readmissions, where the planned readmission occurs before an unplanned readmission, the unplanned readmission does not qualify as a readmission.
In a chain of readmissions, where two or more unplanned readmissions follow an index admission, only the first unplanned readmission qualifies as a readmission. This is because the readmission flag is binary.
Data Dictionary
readmission_summary
The readmission_summary table is at the encounter grain, but we exclude encounters having data quality problems preventing them from being used in readmission analytics. So this table has a subset of the encounters in the encounter_augmented table. For every encounter in this table (i.e. for every row in this table), we have columns representing data elements associated with the encounter as well as data elements associated with a potential readmission encounter. This is the table that is used to calculate readmission rate.
Primary Key:
- encounter_id
Foreign Keys:
- encounter_id (join to core.encounter)
- person_id (join to core.patient)
| Column Name | Data Type | Primary Key | Description |
|---|
encounter_augmented
The encounter_augmented table is at the encounter grain (i.e. each row represents a unique acute inpatient encounter from the core.encounter table). Use this table to look at all acute inpatient encounters and see the data elements associated with each encounter that are relevant for doing readmission analytics. The table also has data quality flags that indicate if each encounter (i.e. each row in this table) qualifies to be used for readmission analytics as well as the different data quality problems for which the encounter might be excluded from being used in readmission analytics.
This table includes columns for data quality tests related to readmissions, so you can see why admissions that are not in readmission_summary were excluded.
Primary Key:
- encounter_id
| Column Name | Data Type | Primary Key | Description |
|---|
Example SQL
Overall Readmission Rate
-- The numerator is the number of encounters that are index admissions
-- (i.e. that are eligible to have a readmission count against them)
-- and DID have an unplanned 30-day readmission:
select
(select count(*)
from readmissions.readmission_summary
where index_admission_flag = 1 and unplanned_readmit_30_flag = 1) * 100
/
-- The denominator is the number of encounters that are index admissions
-- (i.e. that are eligible to have a readmission count against them):
(select count(*)
from readmissions.readmission_summary
where index_admission_flag = 1) as overall_readmission_rate
30-day Readmission Rate by Month
with readmit as
(
select
to_char(discharge_date, 'YYYYMM') as year_month
, sum(case when index_admission_flag = 1 then 1 else 0 end) as index_admissions
, sum(case when index_admission_flag = 1 and unplanned_readmit_30_flag = 1 then 1 else 0 end) as readmissions
from readmissions.readmission_summary
group by to_char(discharge_date, 'YYYYMM')
)
select
year_month
,index_admissions
,readmissions
,case when index_admissions = 0 then 0 else readmissions / index_admissions end as readmission_rate
from readmit
order by year_month
30-day Readmission Rate by MS-DRG
with readmit as
(
select
rs.ms_drg_code
,drg.ms_drg_description
, sum(case when index_admission_flag = 1 then 1 else 0 end) as index_admissions
, sum(case when index_admission_flag = 1 and unplanned_readmit_30_flag = 1 then 1 else 0 end) as readmissions
from readmissions.readmission_summary rs
left join terminology.ms_drg drg on rs.ms_drg_code = drg.ms_drg_code
group by
rs.ms_drg_code
,drg.ms_drg_description
)
select
ms_drg_code
,ms_drg_description
,index_admissions
,readmissions
,case when readmissions = 0 then 0 else readmissions / index_admissions end as readmission_rate
from readmit
order by index_admissions desc
Disqualified Encounters
Let's find how many encounters were disqualified.
select count(*) encounter_count
from readmissions.encounter_augmented
where disqualified_encounter_flag = 1
Disqualification Reason
We can see the reason(s) why an encounter was disqualified by unpivoting the disqualification reason column.
with disqualified_unpivot as (
select encounter_id
, disqualified_reason
, flagvalue
from readmissions.encounter_augmented
unpivot(
flagvalue for disqualified_reason in (
invalid_discharge_disposition_code_flag
, invalid_ms_drg_flag
, invalid_primary_diagnosis_code_flag
, missing_admit_date_flag
, missing_discharge_date_flag
, admit_after_discharge_flag
, missing_discharge_disposition_code_flag
, missing_ms_drg_flag
, missing_primary_diagnosis_flag
, no_diagnosis_ccs_flag
, overlaps_with_another_encounter_flag
)
) as unpvt
)
select encounter_id
, disqualified_reason
, row_number () over (partition by encounter_id order by disqualified_reason) as disqualification_number
from disqualified_unpivot
where flagvalue = 1